Tales from our Women's Health Hub
Urinary incontinence (UI)—the involuntary leakage of urine—is a common issue for midlife women. This A-Z guide explores the causes, treatments, and lifestyle changes that can help manage the condition.
39% of women reported urinary incontinence in a survey of 1,415 women in the UK. (Cooper et al, 2015) but as a woman’s health GP, I feel that urinary incontinence issues are significantly under-reported, as women are too embarrassed to tell anyone. In my clinic I hear about symptoms affecting more than 50% of my patients.
Understanding incontinence through a patient's eyes
A 51-year-old woman came in for a Women’s Health Check with us at The McIndoe Centre and described urinary incontinence.
“My life feels so limited now,” she said. “I am scared of sneezing, coughing or even laughing as I could wet myself. Once it starts it gushes out of me.”
Ever since this patient had a difficult forceps delivery with her last baby 11 years ago, she had been unable to exercise like she used to as she started to notice that her underwear and gym gear would be sodden and smelling of urine. Then during her menopause, she had noticed the episodes of urinary incontinence worsening.
Her life changed the first time she wet herself getting out of her husband’s car—she couldn’t stop it. From that moment, everything became a struggle. She avoided sheer fabrics because incontinence pads were too visible, which made finding gym clothes nearly impossible. She stopped exercising, gained weight, and lost her self-confidence.
Urinary leakage also disrupted her work and social life. She avoided going to the London office because, by lunchtime, the smell became noticeable, and she had to carry spare clothes everywhere. Over time, she withdrew from others, stopped going out, and became increasingly depressed.
She added: “The weight started piling on, and coupled with my urinary leakage, it had a massive knock on effect of my self confidence and put an end to my sex life. I did go to the GP who arranged some investigations but he told me that there were no concerning features and recommended pelvic floor exercises and to lose some weight.”
An A-Z overview of incontinence
This A-Z guide provides a comprehensive overview of the key aspects of incontinence, helping you navigate its causes, symptoms, types, and management options.
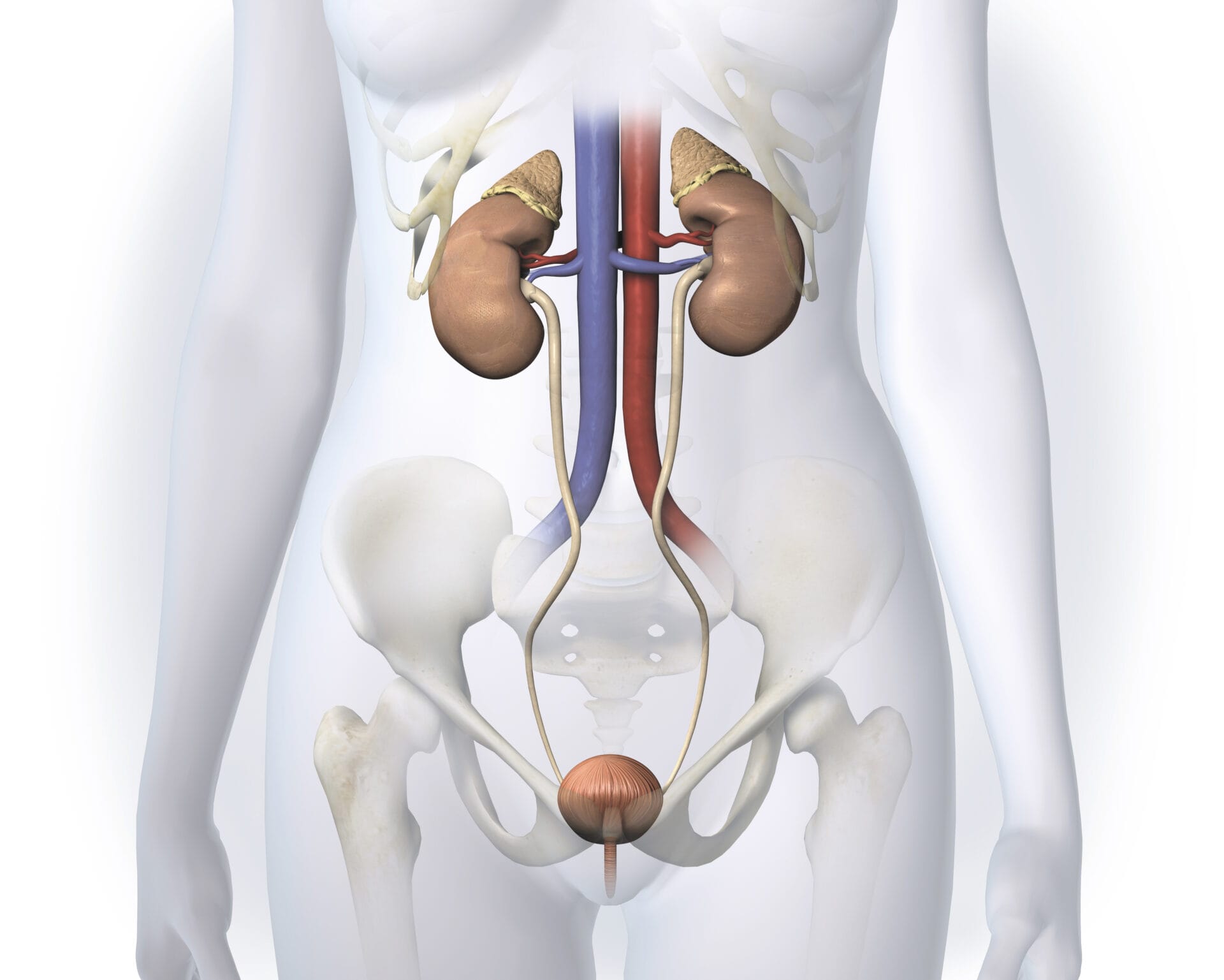
A - Anatomy and physiology of UI
UI often results from changes in the urinary system, which includes the kidneys, bladder, ureters, and urethra. The bladder stores urine, while muscles and nerves control its release. Aging, childbirth, and hormonal shifts can disrupt this system, leading to leakage.
As women age, the bladder's capacity and control mechanisms weaken. This can result in urge incontinence (a sudden, intense need to urinate) or stress incontinence (leakage triggered by physical activity).
B - Bladder dysfunction
Bladder dysfunction is a key contributor to urinary incontinence in midlife women. As women age, the bladder’s capacity to hold urine decreases, and bladder control mechanisms weaken. This can lead to both urge incontinence and stress incontinence.
C - Childbirth and pelvic floor damage
Childbirth, particularly vaginal deliveries involving forceps, prolonged labour, or large babies, can damage pelvic floor muscles and nerves. This reduces bladder support, increasing the likelihood of incontinence.
D - Diabetes and UI
Diabetes can damage bladder-controlling nerves (diabetic neuropathy), leading to urge incontinence or overflow incontinence, where the bladder cannot empty fully, causing leaks.
E - Estriol (oestrogen) deficiency and menopause
Perimenopause and menopause can significantly impact urinary health as oestrogen levels drop. Oestrogen supports urinary tract tissues; and its decline weakens these tissues, reducing elasticity and increasing the risk of incontinence. The decrease in oestrogen levels weakens pelvic floor muscles and affects the bladder’s function, leading to increased incidence of urinary incontinence.
F - Fluid intake
Overconsumption of fluids, caffeine, alcohol, or artificial sweeteners can worsen UI. Balance is essential to prevent dehydration or excessive urine production.
G - Genetics
A family history of UI can increase susceptibility due to inherited traits like weak pelvic floor muscles or connective tissue issues.
H - Hormone Replacement Therapy (HRT)
Oestrogen helps maintain the health of the tissues in the urinary tract, including the bladder and urethra. Topical oestrogen (creams, and pessaries) can be applied directly to the vagina and this acts locally to strengthen urethral tissues, especially post-menopause.
I - Infections
Urinary tract infections (UTIs) are a common temporary cause of UI. They irritate the bladder, triggering urgency and frequent urination.
J - Judgment in treatment
Proper treatment requires identifying the underlying cause of UI. Options include medications, lifestyle changes, and advanced therapies tailored to the individual.
K - Kegel exercises
Kegel exercises strengthen the pelvic floor muscles, which support the bladder. Regular practice can significantly improve stress incontinence.
L - Lifestyle modifications
Maintaining a healthy weight, avoiding bladder irritants, and quitting smoking are critical steps in managing UI.
M - Medications
Several medications target UI symptoms:
- Anticholinergics reduce bladder contractions for overactive bladder.
- Beta-3 agonists relax the bladder, increasing storage capacity.
- Alpha-blockers relax urethral muscles to ease bladder emptying.
N - Neuromodulation therapy
This treatment uses electrical impulses to stimulate nerves controlling bladder function. Sacral neuromodulation is particularly effective for urge incontinence.
O - Obesity
Excess weight places additional pressure on the bladder and pelvic floor, exacerbating UI. Weight loss through diet and exercise often reduces symptoms.
P - Physiotherapy
Pelvic floor physiotherapy combines exercises, biofeedback, and manual techniques to strengthen muscles supporting the bladder. It’s particularly effective for stress incontinence.
Q - Quality of life
UI can deeply affect a woman’s mental health, causing anxiety, embarrassment, and isolation. Counselling and support groups can help address these emotional challenges.
R - Risk factors
Age, obesity, smoking, chronic coughing, and certain medications (like diuretics) all increase UI risk. Awareness allows for preventive measures.
S - Surgical options
For women whose symptoms do not improve with conservative treatments, surgical procedures such as sling surgery, bladder neck suspension, or Botox injections may provide relief.
T - Timing and symptom management
Bladder training and scheduled voiding are effective strategies for improving bladder control over time.
U - Urge incontinence
Characterised by sudden, uncontrollable urges to urinate, urge incontinence can be managed with bladder training, medications, and lifestyle adjustments.
V - Vaginal atrophy
Thinning and dryness of vaginal tissues, common post-menopause, can contribute to UI. Oestrogen therapy may alleviate symptoms.
W - Weight management
Maintaining a healthy weight reduces pressure on the bladder and improves pelvic muscle function, helping alleviate UI.
X - X Factors
Rare causes of UI include neurological disorders (like multiple sclerosis), stress, and medications. Proper diagnosis is essential for targeted treatment.
Y - Yoga
Yoga strengthens pelvic floor muscles, promotes relaxation, and reduces stress, supporting bladder control and overall well-being.
Z - Zero tolerance for neglect
Ignoring UI can worsen symptoms and affect quality of life. Timely treatment, ranging from lifestyle changes to advanced therapies, can provide significant relief.
By understanding these aspects of UI, midlife women can take control of their health and explore effective solutions tailored to their needs.
Relief through targeted treatment
Dr Sloan adds: "As a result of spending time with the case study patient during her women’s health check, we were able to help her by recommending a medication to help her overactive bladder and some hormonal oestrogen cream to support her urethral health. We wrote to her GP and asked for these medications to be added to her NHS prescription. After she got her bladder control back, she was able to focus on her lifestyle changes – she resumed the gym and joined a yoga class. She is now focusing on her nutrition and is already starting to lose some weight. This will really benefit her overall health and help her to get her self-confidence back."
A path towards confidence and comfort
In conclusion, urinary incontinence is a common issue among midlife women, often resulting from a combination of anatomical, hormonal, and lifestyle factors. Understanding the causes and treatment options, including medications, physiotherapy, lifestyle changes, and even surgical interventions, is crucial for managing and overcoming the condition. With the right approach, many women can significantly improve their symptoms and regain control over their bladder function.
Book a Women's Health Check at The McIndoe Centre
We believe preventive care and early detection of health risks are key to long-term wellness. Our comprehensive assessment covers a broad spectrum of women’s health tests, all conducted on the same day, to provide an overview of your health status.
Take charge of your wellbeing and book an appointment with one of our GP and Women's Health Specialists at The McIndoe Centre.
News and articles
We offer a range of news and blog articles to enable people to make more informed decisions when it comes to the treatments we have at The McIndoe Centre.







